In 2025, the European Union began developing bloc-wide mechanisms to coordinate the supply of medicines. Plans include expanding production, organizing joint procurement, and attracting new pharmaceutical companies to the market. The move came in response to the growing number of critical drug shortages affecting Europe’s healthcare systems, with pharmacists reporting that dozens of medicines can be unavailable at the same time. The disruptions stem from shortcomings in government regulation, weak communication between countries, and the fragmentation of the European market. According to experts, the measures introduced to combat shortages have not been swift enough to resolve the problem.
Content
Everything is there – yet nothing is available
What qualifies as a shortage?
Drug shortages through the eyes of pharmacists
How shortages arise
Main causes of disruptions
Attempts to address the problem
A course toward stability
Everything is there – yet nothing is available
In January 2023, France’s National Agency for the Safety of Medicines (ANSM) reported serious supply problems with antibiotics, particularly amoxicillin. The most acute shortages affected formulations such as oral suspensions, which are used to treat infectious diseases in children. The government directed that existing reserves be redistributed to pharmacies to ensure a more even supply across the country.
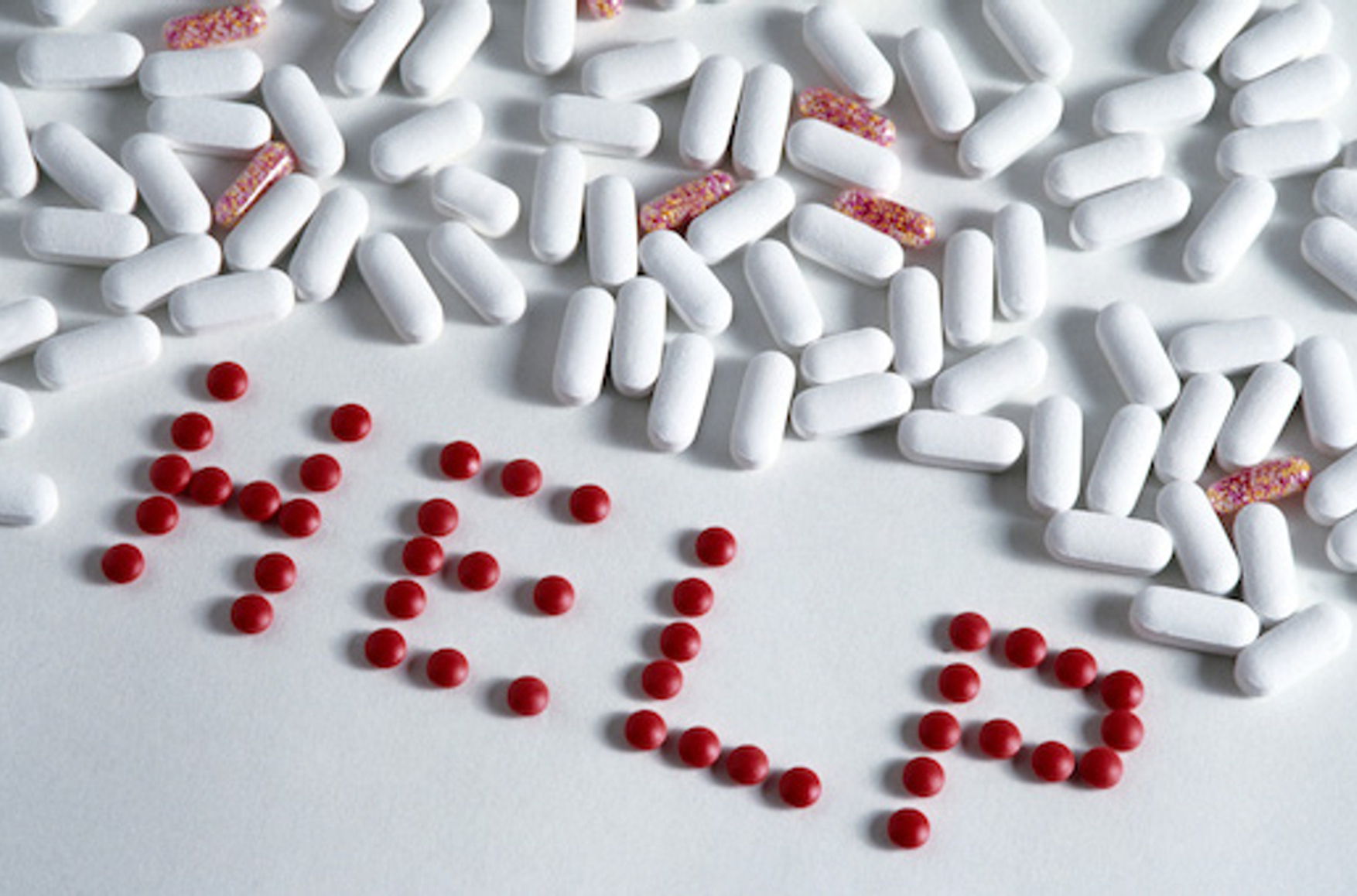
In recent years, drug shortages have become a persistent problem for healthcare systems continent wide. At present, the European Union is a global leader in regulating the pharmaceutical market, yet it is increasingly confronted with the physical absence of medicines precisely when they are needed most. When shortages occur, patients and clinics pay it in waiting time, additional risks, and reduced quality of treatment.
“Cases of medicine shortages are regularly recorded across the European Union. Their frequency and severity reached record levels in 2023–2024. This situation creates difficulties for patients, places additional strain on healthcare systems, and highlights the EU’s strategic vulnerability in medical supply,” Klaus-Heiner Lehne, the former president of the European Court of Auditors, said in September 2025.
What qualifies as a shortage?
Regulators distinguish between different types of medicine shortages. A standard shortage refers to the temporary unavailability of a drug in a particular country or from specific suppliers. Such situations are usually caused by local factors like production disruptions or problems with logistics and packaging. In these cases, the gap can typically be addressed by dipping into existing stockpiles, making purchases from alternative brands, or substituting therapeutically equivalent medicines.
A critical shortage, by contrast, arises when a medicine is unavailable in several countries at once and, crucially, no adequate alternative exists — either because the drug is completely irreplaceable or because substitutes are clinically insufficient for some patients. Addressing this type of shortage requires cross-border coordination: joint redistribution of stock, collective procurement, or emergency regulatory measures.
From January 2022 through October 2024, the European Medicines Agency (EMA) recorded 136 cases of critical medicine shortages — situations in which countries were unable to ensure access to specific drugs or find alternatives without coordination at the EU level.
Drug shortages through the eyes of pharmacists
A 2025 report published by the European Association of Hospital Pharmacists (EAHP) documents the systematic impact of medicine shortages on clinical practice: “Eighty-nine percent of pharmacists consider shortages a serious problem. This assessment is shared by 84% of physicians, 68% of nurses, and 86% of other healthcare workers.”
The report lists the consequences of supply disruptions:
• 59% of respondents said shortages led to delays in treatment,
• 43% said they resulted in the selection of less-than-optimal therapies,
• 35% said they left patients without care.
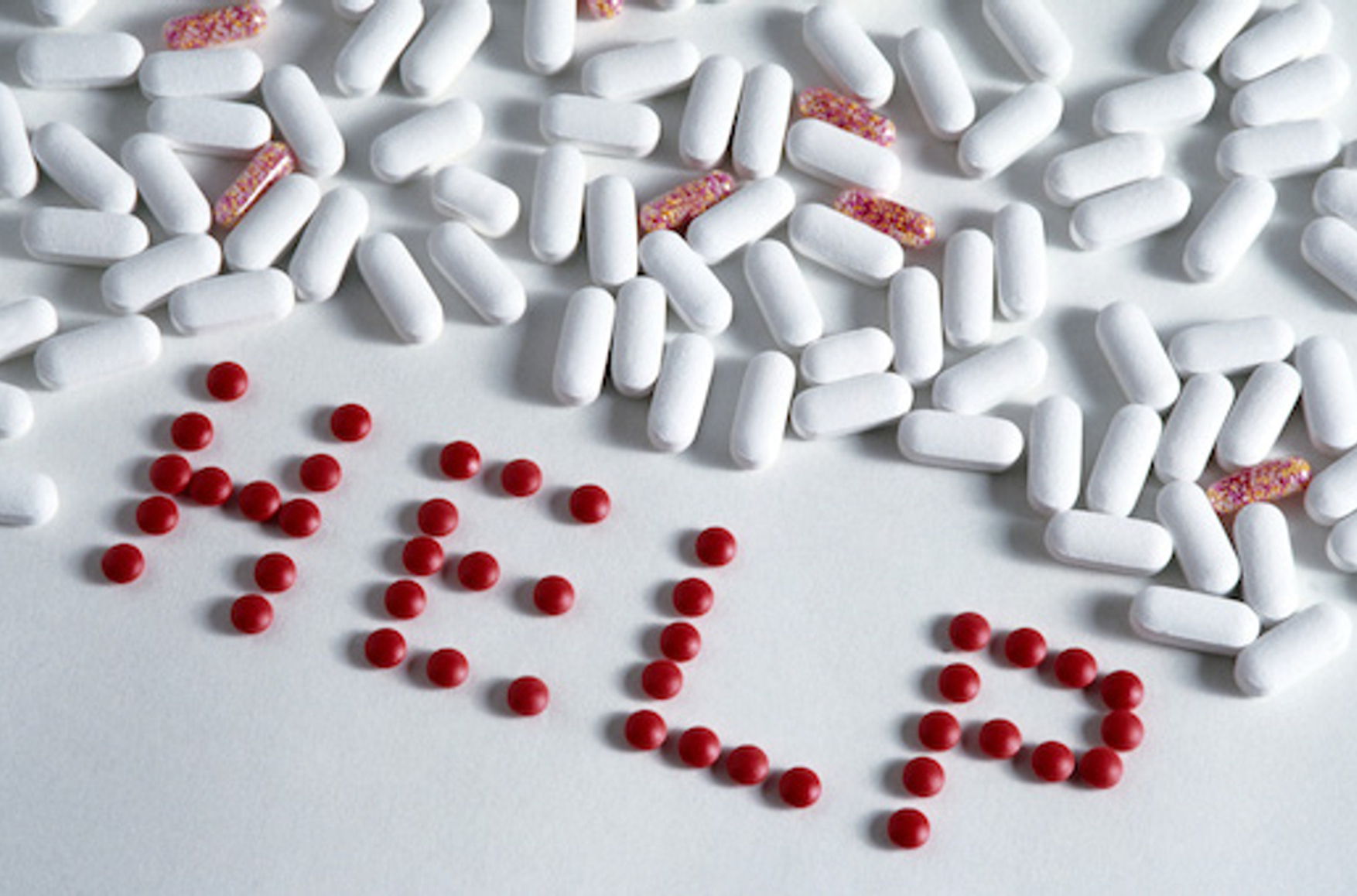
The study also offers a “portrait of the crisis” by drug class. In 2023, the medicines most frequently reported as being in short supply were antibiotics, painkillers, and anesthetics (including narcotic agents). These groups form the backbone of standard treatment protocols and emergency care, amplifying the impact of shortages on patient outcomes and hospital infrastructure.
Antibiotics, painkillers, and anesthetics (including narcotic agents) were most frequently cited as the medicines in short supply
As a result, clinical pharmacists are forced to spend time managing logistics in order to cope under conditions of limited stock. This reduces the quality of care for hospitalized patients, who are already facing a lack of necessary medicines. Overall, the European medical community views shortages as an extremely serious problem for healthcare systems.
How shortages arise
The system for supplying medicines to clinics can be compared to a funnel with limited capacity. The active pharmaceutical ingredient is produced at a small number of facilities, then sent to plants where finished forms are manufactured. From there, it passes through the marketing authorization holder and distributors before finally reaching hospitals or pharmacies. A disruption at any stage of this process is immediately felt by the end user.
A disruption at any stage of the process is immediately felt by patients
The main difficulty lies in collecting and transmitting information. To respond quickly to supply disruptions, national and EU-level regulators must receive timely signals from all market participants. Data need to be submitted in a unified format so they can be combined into a coherent overall picture.
At present, notifications reach both regulators and pharmacists from various sources, with differing levels of detail and on different timelines. An understanding of how much stock remains and what alternative options exist usually emerges only when supplies are coordinated manually.
In a special report published in 2025, the European Court of Auditors points to inconsistencies in the format of notifications about potential supply disruptions and to fragmented data on medicine stockpiles. Too often, information about a drug shortage arrives too late for an optimal response to be developed.
When that happens, doctors and pharmacists are forced to seek alternatives, redistribute supplies, and revise treatment regimens under tight deadlines — all while relying on incomplete data. Shortages are shaped by the supply chain itself: market conditions change faster than information is updated.
Main causes of disruptions
Breakdowns that lead to shortages can occur at any point in the supply chain — from the production of active pharmaceutical ingredients to retail distribution, areas where legislative and market constraints can further complicate matters.
The founding document of the Critical Medicines Alliance, established by the European Commission in order to analyze vulnerabilities in pharmaceutical manufacturing, explicitly states the need to identify and eliminate weak links in supply chains. Particular attention is paid to medicines of priority importance — those for which dependence on a small number of active ingredient manufacturers makes the market more sensitive to disruptions.
Production and quality control
A 2022 report by the Pharmaceutical Group of the European Union identified the main causes of shortages as “disruptions or suspension of the manufacturing process, the introduction of production quotas at facilities, and unexpected increases in demand for medicines, including pediatric antibiotic formulations.”
Disruptions often occur after inspections reveal deviations from standards. When that happens, companies must pause production, recall finished batches, or shut down specific production lines.
Shortages can also result from the revision of registration dossiers, tighter impurity controls, and updated pharmacovigilance criteria. These changes often require technical upgrades at manufacturing sites, and additional requirements may make the production of low-cost medicines less economically viable.
Availability of pharmaceutical substances
A second source of vulnerability is the production of active pharmaceutical ingredients (APIs), which are manufactured in only a few regions. A disruption at this level automatically affects the availability of the final product across the EU.
The vulnerability of pharmaceutical supply chains at the API stage is noted in a European Commission comment regarding the EU’s dependence on imported medicines and substances. Some drugs and their components are supplied to the EU from third countries because European production capacity is insufficient, and as a result, any disruption to imports can lead to shortages.
Procurement and pricing
Another cause of shortages is government control over drug prices. In most EU countries, medicines are purchased through reference pricing systems and tenders, where the lowest bid wins. For widely used basic medicines, this model leads to sustained margin compression. Over time, some manufacturers exit the segment, and supply becomes concentrated in the hands of a limited number of players.
The pharmaceutical community describes state price regulation — alongside production disruptions — as one of the key causes of medicine shortages. A focus on the lowest price reduces incentives for new suppliers to enter and for companies to build up buffer stocks, and when supply depends on only one or two players, even a local setback quickly becomes a sector-wide problem.
National barriers
Policy discrepancies also play a role. Even if a medicine has received EU-wide marketing authorization, this does not guarantee that it will actually be available for sale in all member states. National markets remain under the authority of local governments, which regulate everything from labeling and packaging requirements to commercial launch. As a result, countries compete for supplies rather than offsetting each other’s shortages.
Even if a medicine has received EU-wide marketing authorization, this does not mean it will actually be available for sale in all member states
When a drug is physically available in one country, selling it in another requires regulatory approval, repackaging, or other additional procedures, which can significantly slow the process even amid a shortage. A report by the European Court of Auditors states that “fragmentation of the pharmaceutical market in the EU hampers the free circulation of medicines and leads to unequal access to them.”
Parallel trade
In times of shortage, a straightforward market mechanism comes into play: medicines are supplied to places where prices and margins are higher, meaning that countries with stricter regulation are left with empty shelves. For example, during Greece’s debt crisis in 2012, the authorities imposed a ban on the export of all medicines in an attempt to keep them in the country. The result was that manufacturers directed most of their products to more profitable markets, meaning that drugs were simply not imported into Greece in sufficient quantities.
In recent years, pharmaceutical companies have reduced production in Europe, shifting capacity to countries where manufacturing is cheaper and profit margins on final sales are higher. In September 2025, Eli Lilly CEO Dave Ricks said that due to tight pricing regulation, the United Kingdom is becoming less attractive to investors and suppliers and therefore receives new medicines later than more open markets like the United States do.
Pharmaceutical companies have reduced production in Europe, shifting capacity to countries where manufacturing is cheaper and profit margins are higher
The rules governing parallel trade — when a product sold at a lower price in one country is resold by dealers in another at a higher price — lack transparency. Pharmacists often do not understand how such imports are regulated, and as a result, even during shortages medicines continue to flow to markets where they can be sold at higher prices. Healthcare systems in countries with lower-priced medicines are vulnerable due to the fact that they are the last to be resupplied in the event of a shortage.
Stockpiling
The creation of medicine reserves in the European Union is also regulated at the national level, and standards can vary significantly. Differences concern the lists of reserve medicines, the size of stockpiles, and storage periods. Coordination between countries in these areas remains weak.
During periods of shortage, governments act in the interests of their own healthcare systems, keeping medicines within their borders and building up reserves. There is no unified European mechanism to coordinate such decisions. As a result, while stockpiles are seen as a safeguard at the national level, shortages emerge at the EU level.
Attempts to address the problem
In recent years, EU regulators have sought to build a system of early response, prioritization, and coordination in order to adopt not only targeted but also comprehensive measures aimed at countering shortages. In 2022, an EU regulation assigned the European Medicines Agency (EMA) responsibility for monitoring supplies and coordinating action during crises (including epidemics and large-scale production or logistics disruptions). The agency was given a mandate to collect data on medicine availability, assess risks, and activate EU-wide response mechanisms.
For these purposes, the European Shortages Monitoring Platform (ESMP) was established. It began operating in 2024, and its powers were subsequently expanded. The platform will aggregate notifications from manufacturers, distributors, and public authorities in a standardized format in order to identify shortage risks at an earlier stage.
In addition, the EU launched a network of National Contact Points, known as the Shortages Single Point of Contact (SPOC). This system creates a channel for cross-border communication during supply disruptions. Each member state has established a contact center through which national regulators transmit information on shortage risks to the EMA and receive coordination guidance.
The next element is the creation of a pan-European list of priority medicines. The “Union list of critical medicines,” established by the EMA, sets the focus for monitoring and helps direct resources toward drugs that are essential to the stability of clinical practice.
However, EU auditors point to the limitations of these mechanisms. Materials from the European Court of Auditors emphasize that for a long time the EMA had only fragmented data on shortages and, outside of crisis situations, operated with limited powers.
A course toward stability
The European Union is gradually changing its approach to securing medicine supplies. In March 2025, the European Commission introduced the Critical Medicines Act — a direct response to growing supply disruptions and the continent’s heavy reliance on imports. The proposed legislation calls for expanding domestic production, attracting new suppliers, and creating EU-wide coordination mechanisms. Priorities include the establishment of long-term contracts, joint procurement arrangements, and support mechanisms for companies willing to invest in reserve capacity.
Success will be measured by the change (or lack thereof) in the frequency of critical shortages, the consolidation of the market, and the emergence of real economic incentives to sustain production and attract new suppliers. In December 2025, the EU Council agreed on a common position, sending a clear political signal that national strategies to combat shortages are being consolidated into a unified European framework.